Dysthymia, known in the ICD-10 as F34.1, is also called Persistent Depressive Disorder (PDD). It isn't a sudden storm of sadness but more like a long, overcast day that never seems to clear. This persistent, low-grade depression can quietly affect your energy and ability to feel joy.
Understanding Dysthymia and the ICD-10 Code F34.1
Have you ever felt like you're just going through the motions, with life's colours turned down? That's a common way people describe living with dysthymia. It’s less about intense sadness and more about a persistent feeling of being "down."
The official code, dysthymia ICD 10 F34.1, helps mental health professionals classify this condition. This universal code ensures that whether you're in Mumbai or London, clinicians share a common language for care. It helps validate those subtle but draining feelings that are often dismissed as just a "bad mood."
The Role of ICD-10 in India
In India, healthcare professionals use the ICD-10 framework to recognise dysthymia as a long-term depressive disorder. A key indicator is a persistent low mood that has lasted for at least two years. This system is vital for coding the condition within India's mental health services, from local clinics to national hospitals.
This framework supports India's National Mental Health Programme, guiding clinicians in their assessments and ensuring consistent care.
It’s so important to remember that these feelings are not a personal failing or something to just "get over." Understanding your experience is a starting point for finding the right path to feeling better.
Recognising these persistent symptoms can help you find relief and rediscover a life with more purpose. It empowers you to address challenges like workplace stress and anxiety and start building resilience for a brighter future.
To help break it down, here’s a quick overview of the key ideas we’ve discussed.
Dysthymia (F34.1) at a Glance
| Concept | Simple Explanation |
|---|---|
| Dysthymia | A long-term form of depression with less severe but more persistent symptoms. |
| ICD-10 Code F34.1 | The official code used by healthcare professionals worldwide to identify dysthymia. |
| Key Symptom | A persistent low mood that lasts for at least 2 years in adults. |
| Common Feeling | Often described as feeling like you're living in "grayscale" or are constantly in a funk. |
| Importance of Clarity | Validates your experience and opens the door to effective support and well-being strategies. |
This table shows that while the terms might seem clinical, the experience is deeply human. Recognizing these patterns is a compassionate first step toward seeking support.
Recognising the Subtle Signs of Dysthymia

It can be easy to mistake dysthymia for a personality trait because its signs are quiet and relentless. People living with it may feel it's just "who they are," which is why it's so important to recognise.
This isn't just about a clinical checklist; it’s about the reality of getting through the day. Imagine a constant fatigue that a full night's sleep can't touch, making every small task feel like a challenge.
How Dysthymia Shows Up in Daily Life
This ongoing, low-grade depression can appear in ways that are easy to brush off. You might notice persistent patterns that affect your daily life and sense of well-being.
- Difficulty concentrating: Your mind might feel foggy, making it tough to stay focused at work or in conversations.
- Feelings of hopelessness: A gloomy outlook can cast a shadow over everything, making it hard to feel positive about the future.
- Changes in appetite or sleep: You might overeat or have no appetite at all, or perhaps you sleep too much or too little. It's a long-term pattern, not just a bad week.
The key element is duration. For an assessment, these feelings need to have been present for at least two years in adults. This persistence is why it can be mistaken for pessimism, but what you're feeling is real, has a name, and is not something you have to live with.
Dysthymia in the Indian Context
In India, the pressures of modern life, especially in urban centres, can contribute to conditions like dysthymia. The unique stressors of city living, from career pressures to social demands, can take a toll on mental well-being. For more information, you can explore some insights on dysthymia documentation.
Simply putting a name to these feelings is a powerful first step. It validates your struggle and opens the path to support through counselling or therapy. The right guidance can help you build resilience and reclaim your sense of well-being. Please remember, assessments are for informational purposes, not for self-diagnosis.
It's helpful to understand the difference between dysthymia and major depression to find the right support. A simple weather analogy can make this clearer.
Imagine dysthymia as a persistent, gloomy drizzle that lingers for years. It's not a torrential downpour, but it's constant enough to leave you feeling damp and down. You can still go about your day, but that grey cloud is always there.
Major depression, on the other hand, is like a sudden, intense thunderstorm. It can feel overwhelming and make it difficult to do much of anything, though these storms are typically shorter in duration.
Differentiating for Clarity
The main differences are duration and intensity. Medically, dysthymia is classified under the ICD-10 code F34.1, and a core criterion is its long-term nature. An adult must experience a low-grade depressed mood for at least two years. Major depression is identified by more severe symptoms that disrupt life over a shorter period, usually at least two weeks.
Sometimes, a person living with the constant drizzle of dysthymia can also experience a major depressive thunderstorm. This is often called "double depression" and requires a thoughtful approach in therapy or counselling.
Dysthymia vs Major Depression: A Simple Comparison
This table helps clarify the core differences, focusing on how duration and intensity play out for each condition.
| Feature | Dysthymia (PDD) | Major Depression (MDD) |
|---|---|---|
| Duration | Long-term, lasting at least 2 years for adults. | Episodic, lasting at least 2 weeks. |
| Symptom Intensity | Less severe but persistent and nagging. | Intense, often disruptive symptoms. |
| Typical Description | A constant "low" or "empty" feeling. | Overwhelming sadness and loss of interest. |
Seeing them side-by-side highlights that while they involve similar feelings, their impact unfolds differently over time.
This visual guide offers another way to understand the main differences, focusing on the timeline and the severity of the symptoms.
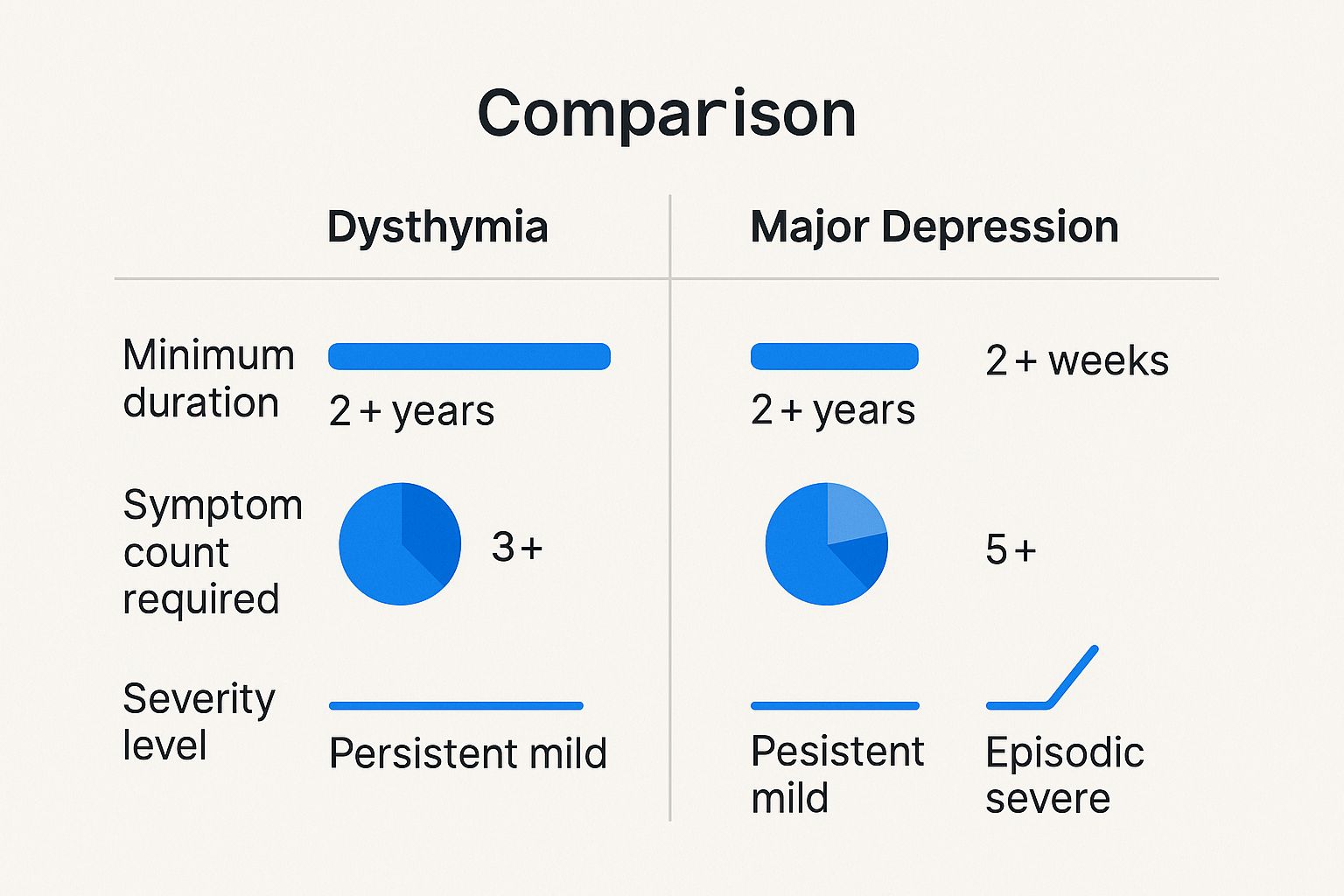
As the infographic shows, dysthymia is a marathon of low mood, not a sprint. Its challenge lies in its persistence.
Understanding this isn't just about labels; it's about validation. It helps explain why the ongoing weight of workplace stress or general anxiety can feel so heavy. Armed with this clarity, you can seek the right support to build resilience and enhance your well-being.
Please keep in mind that this information is for educational purposes only. An assessment from a qualified professional is always recommended for diagnostic clarity.
The Slow Burn of Dysthymia on Daily Life

Living with dysthymia can feel like trying to run a marathon with weights on your ankles. It isn't a sudden crisis but a slow, relentless drain on your energy that quietly impacts your quality of life. Over time, this constant low mood makes everyday challenges feel heavier, affecting everything from relationships to work.
This persistent emotional weight can create a cycle of workplace stress and anxiety. When you're always feeling drained, deadlines can seem overwhelming and social interactions can become exhausting. Exploring supportive tools like work-from-home productivity tools might offer practical ways to manage responsibilities.
How It Affects Well-Being and Resilience
The long-term nature of dysthymia can make it difficult to feel genuine joy or happiness. Moments that should be happy can feel flat, making it harder to connect with loved ones. This can lead to a sense of isolation, even when you’re surrounded by people.
According to the ICD-10, dysthymia (F34.1) is identified by a depressed mood lasting at least two years. Its symptoms are less severe than major depression but are much more persistent. In India, this experience is common, especially among adults in urban areas facing intense professional and personal pressures.
This is where positive psychology can offer a path forward. Building resilience is not about pretending you don't have bad days. It’s about learning to navigate those feelings with more self-compassion, shifting the focus to nurturing your overall well-being.
Shifting Toward Hope and Self-Compassion
Making small, positive changes can make a big difference. The journey is often about cultivating a gentler relationship with yourself and finding pockets of happiness and peace.
- Practise Self-Compassion: Acknowledge that your struggle is real and treat yourself with the same kindness you would show a friend.
- Build Resilience: Through therapy or counselling, you can learn coping strategies to better handle life's inevitable ups and downs.
- Find Moments of Connection: Make a conscious effort to seek small, meaningful interactions that can gently lift your spirits.
By focusing on these steady steps, you can begin to loosen the grip that a chronic low mood has on your life and move toward a more hopeful outlook.
Finding Your Path to Professional Support
Reaching out for help is a sign of great strength. Professional therapy and counselling provide a safe, confidential space to make sense of your experiences. This support can help you learn new ways to manage your mental well-being.
Think of it as building an alliance with a trained professional who is on your side. A strong therapeutic relationship, where you feel heard and understood, is key to a positive outcome.
Effective Therapeutic Approaches
Several well-researched therapies can be effective for dysthymia. Each offers a valuable way to work with the chronic low mood associated with a dysthymia ICD 10 code.
- Cognitive Behavioural Therapy (CBT): This practical approach helps you identify and challenge negative thought patterns that contribute to feelings of depression and anxiety. It provides concrete tools to reframe your thinking and build resilience.
- Psychodynamic Therapy: This form of counselling helps you explore how past experiences might be shaping your present emotions. Understanding these patterns can lead to powerful insights and healthier ways of relating to yourself and others.
Therapy is a journey of self-discovery, not a quick fix. It’s your dedicated time to practice self-compassion, manage challenges like workplace stress, and gradually rediscover a sense of hope and happiness.
The best therapy is the one that feels right for you. It can also be helpful to learn about therapeutic communication techniques. Finding the right support is a crucial step on your journey toward a brighter future.
Taking the First Step Toward a Brighter Outlook
Realising that the persistent shadow you've lived under has a name—like dysthymia ICD 10 F34.1—can be a powerful moment. It’s not about a label, but about acknowledging your struggle. This is the first step toward finding self-compassion and effective support.
This new understanding empowers you to shift from feeling stuck toward exploring pathways to a brighter sense of well-being.
The journey forward can begin with small, manageable actions. Sometimes, just talking to a trusted friend or family member can lift an enormous weight.
Another gentle step is reaching out to a mental health professional for an initial chat. Think of it as a conversation to help you both better understand what you've been experiencing.
Remember, this journey is not about finding a quick cure but about building a kinder, more compassionate relationship with yourself. Supportive takeaways and strategies are available, and feeling better is possible, one step at a time.
At DeTalks, we're here to walk alongside you whenever you feel ready. Exploring therapy or counselling can equip you with practical tools to build resilience and better navigate challenges like workplace stress and anxiety. You don’t have to do this alone.
Frequently Asked Questions About Dysthymia
When you've been feeling low for a long time, it's natural to have questions. Let's walk through some common ones about dysthymia to bring some clarity to your experience.
Can Dysthymia Go Away on Its Own?
Because dysthymia is a long-term condition, it rarely resolves without support. You might have better days, but the underlying low mood often returns. The good news is that guidance through therapy or counselling can make a world of difference by helping you build coping skills and improve your overall well-being.
Is Dysthymia Just a Part of My Personality?
This is a common misconception. When you've felt a certain way for years, it's easy to think it's just who you are. But dysthymia is a recognised mood disorder with specific indicators (dysthymia ICD 10 F34.1), not a character flaw. It is a health condition, and a therapist can help you untangle your true self from the symptoms of depression.
What Is the First Step if I Think I Have Dysthymia?
A gentle and effective first step is to have a conversation with a mental health professional. A counsellor or psychologist can listen to your experiences and conduct an assessment for informational purposes. Remember, an assessment is a tool to understand the best way to support you, not to apply a label. Reaching out is an act of strength.
At DeTalks, we offer a safe, trusted space for you to take that first step toward building your resilience. Explore our confidential, science-backed assessments to gain clearer insight into your mental health and connect with a qualified professional who can guide you on your journey.





